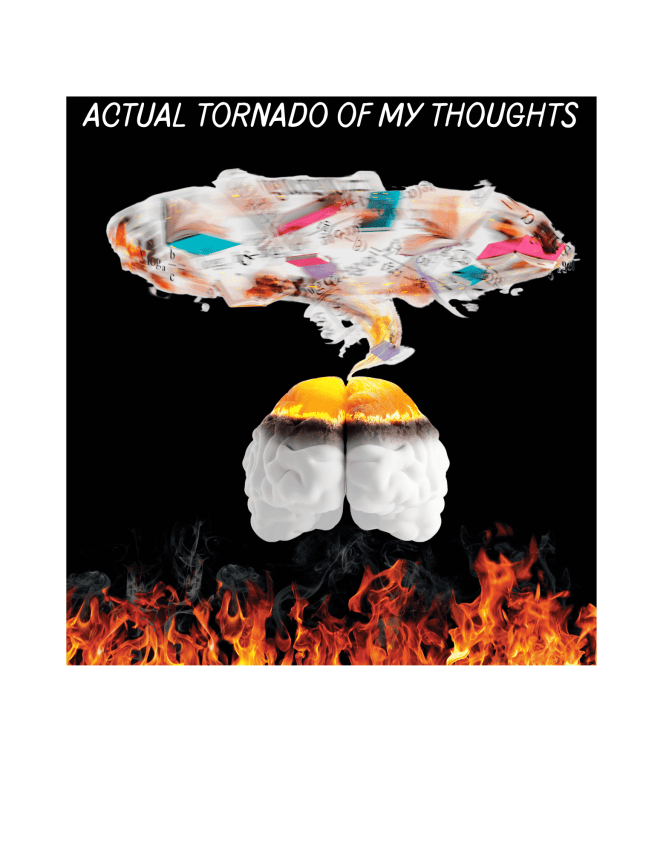
There’s something almost intoxicating about hypomania. Your brain buzzes, ideas come faster than you can write them down, and suddenly everything feels possible. You’re cleaning the garage, starting a new project, texting friends back after weeks of silence, and maybe even feeling like you’ve finally “figured it out.”
But here’s the part people don’t talk about enough: what happens after.
When the sparkle fades and your energy crashes back to earth, you’re left sorting through the emotional and physical wreckage. It’s not just exhaustion—it’s this weird cocktail of regret, confusion, and grief. You might feel raw, embarrassed, or even guilty for things you said or started and couldn’t finish. That aftermath can be brutal.
Hypomania is part of bipolar II disorder—it’s marked by elevated mood, a surge in productivity, and bursts of creativity or restlessness. But while it can feel euphoric at the time, the come-down can leave you reeling, questioning your choices, and trying to clean up the mess your over-caffeinated brain tornadoed through.
The Cycle of Risk and Regret (a.k.a. Oops, I Did It Again — But Not in a Fun Britney Way)
Here’s the thing no one glamorizes about hypomania: the aftermath of impulsive choices that seemed like brilliant ideas at the time. One minute you’re ordering $200 worth of “self-improvement” stuff at 2 a.m., signing up for a new certification course, and texting your ex like you’re starring in your own comeback tour — and the next, you’re wondering what the hell just happened.

And science backs it up. According to research published on PubMed, people in hypomanic states often engage in high-risk behaviors — overspending, substance use, reckless decisions — the kind of things that feel like you’re chasing possibility, but too often watching it all boomerang back with the grace of a collapsing Jenga tower.
What follows? That slow, sinking feeling. Guilt. Shame. Maybe even avoidance. You look at the credit card bill, or a strained relationship, and suddenly the vibrant energy of hypomania gets replaced with the emotional hangover no one warned you about.
You’re not the only one who’s been caught in this loop. You’re not a bad person. You’re a person with a disorder that messes with impulse and inhibition. It doesn’t excuse the consequences, but it does explain the pattern — and understanding the pattern is how we start breaking it. I was so stuck here myself but perhaps worse is the gaslighting I do over EVERY. SINGLE. DECISION. afterwards because I sincerely have lost all faith in my own judgment. Like every little thing, ‘is it a good idea or are you just manic’ plays in my head on a loop.
The Crash Landing No One Talks About
If hypomania feels like flying a little too close to the sun, then the crash that follows is more than just a rough landing — it’s a total freefall. One minute, you’re bursting with ideas and energy, barely sleeping, maybe even reorganizing the garage at 2 a.m. like you’re possessed by the spirit of Marie Kondo on espresso. And then… it’s like the lights shut off. The energy vanishes. You’re not just tired — you’re hollowed out. The sadness is deep, the fatigue bone-heavy, and everything starts to feel like too much and not enough, all at once.
It’s not just a “mood swing.” It’s a full-body, full-mind shutdown that makes even brushing your teeth feel like a high-stakes negotiation. And the cruelest part? The contrast. You remember how you felt just days ago, and now you can’t fathom getting off the couch. That whiplash is its own kind of heartbreak. Like it physically makes me ache sometimes.
When Life Throws a Brick Through the Window
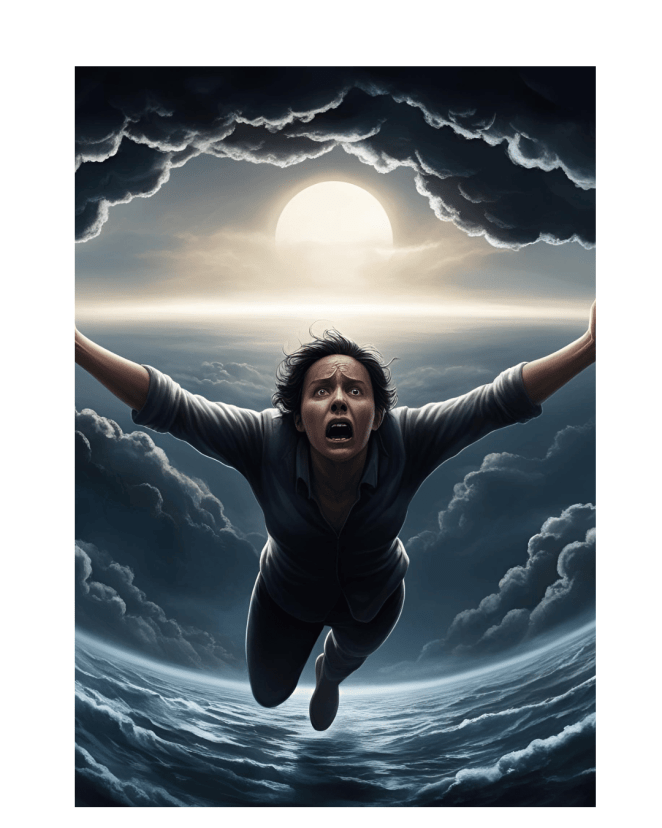
Here’s the thing: if you’re already dancing on the edge of a depressive episode, real-life chaos doesn’t just nudge you — it can send you tumbling. Research backs this up: negative life events (you know, the kinds that seem to show up all at once like uninvited guests) have been shown to intensify depressive symptoms in folks with bipolar disorder [PMC, Cleveland Clinic]. And if you’re someone already wired with a predisposition
to depression? That impact hits even harder. It’s why managing stress isn’t just a suggestion — it’s survival. I will legit cry over such trivial stuff, then hate myself cuz I KNOW its dumb to cry about it so I cry more cuz I’m mad at myself for not being able to look at a situation thats got nothing to do with me or so so trivial Learning how to soften life’s blows, build resilience, and stack the odds in your favor might not make the hard stuff disappear, but it can definitely make it hurt less when it lands.
Moving Forward: Strategies for Coping (AKA, Surviving the Crash Without Losing Your Damn Mind)
Look, managing life after hypomania is like waking up in a house you swore you just deep cleaned, only to find emotional dishes stacked in every room. But there are ways to climb out of the mess — even if you’re doing it one spoon at a time.
🔹 Self-Compassion
This is not a personal failure, a moral shortcoming, or some character flaw you need to apologize for. It’s a medical condition — full stop. Remind yourself (repeatedly, if needed) that what you’re feeling isn’t your fault. You’re not broken, you’re human. In a world that crops all the edges to paint a rosier picture be the straight angle in black and white.

🔹 Structured Support
When your brain feels like a Pinterest board of chaos, routines can become lifelines. Simple, repeatable actions — morning check-ins, meal planning, a therapy appointment every other Tuesday — can help stabilize the rollercoaster. And yes, professional help is allowed and encouraged (therapy = tools, not weakness). Every morning my routine has been the same for years, Duolingo while I listen to stand up comedy with the news in the background, if any of those is missing my day starts out lacking which leads to a bad day
🔹 Community Connection
Even if you’re more “socially exhausted introvert” than “group hug enthusiast,” connecting with people who get it can make a huge difference. Whether it’s an online forum, a group chat, or that one friend who won’t judge your 2 a.m. existential texts — don’t go it alone. Thats what I’m trying to do here, build a community, hopefully to work right on up to a forum we can all support each other. Thats my goal anyway the minute I can sell enough in my store to pay to host the forum it will be done!
Understanding the highs and lows — especially the rough emotional terrain that can follow hypomania — isn’t just helpful, it’s empowering. When you mix solid science with self-awareness and some well-worn coping tools, you start to feel just a little more in control. Not perfect, not invincible — but stronger. And that counts. Til next time gang, take care of yourselves, and each other.
P.S. If this hit a little close to home and you’re looking for something to help you process the messy in-between parts — I made a workbook just for this. It’s not magic, but it’s honest, helpful, and created by someone who’s been there. Check it out