Or: How My Medicine Cabinet Became a Small Pharmacy and I Still Can’t Remember What I’m Supposed to Take When
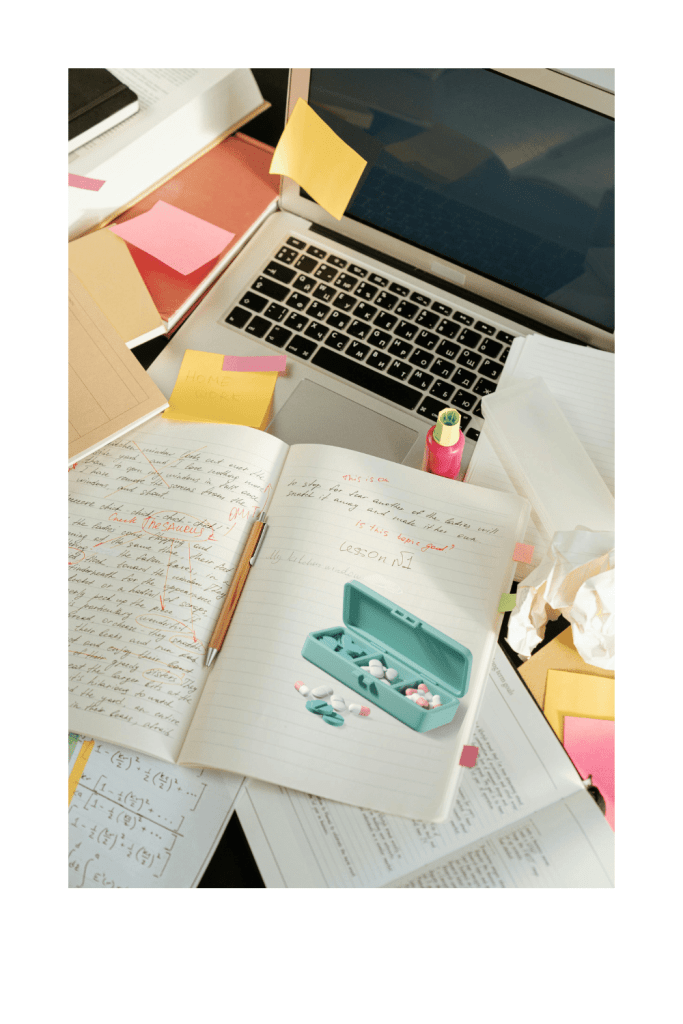
Looking at my bathroom counter right now, I count fourteen different pill bottles, three liquid medications, two inhalers, and a partridge in a pear tree. Okay, maybe not the partridge, but at this point I wouldn’t be surprised if my doctor prescribed one for “mood support.”
For those of you managing multiple chronic conditions, you know the drill. What started as “just take this once a day” has evolved into a complex choreographed dance that would make Broadway jealous. And like any good performance, timing is everything—except I have ADHD and the memory of a goldfish with anxiety.
Meet the Cast of Characters
The Morning Crew: These are the heavy hitters that transform me from zombie to semi-functional human. They’re the ones that make it possible for me to remember my own name and possibly locate the coffee maker.
I have to take 16 pills in the morning, and it’s as gross and exhausting as it sounds. While I’m supposed to take all that in the morning, I split it up to make it easier to manage, so my pills are morning, later morning, dinner/bed. Frequently when I sit down to do my meds I have missed a few from the “later morning” category. Because nothing says “good morning” like swallowing what feels like a handful of gravel.
The Evening Squad: The night shift workers whose job is to help me actually sleep instead of lying awake cataloging every embarrassing thing I’ve done since 1987.
At night I feel like I do a lot of prep work. I take 5 at dinner. One of those is half a dose of sleep/anti-anxiety. I take another 3 when I sit down for the night. Once I have done my chores I pop the other half and soon am out cold. If any one of those is off by an inch I won’t sleep or will pass out mid-chore. It’s like a tightrope balance really, but I fall far more often lol. Nothing quite like waking up on the couch with a half-folded load of laundry as your blanket.
The Wildcards: These are the divas of the medication world. Take with food. Don’t take with food. Take two hours before this other medication but not within four hours of dairy products. Take while standing on your head during a full moon. (Okay, I made that last one up, but honestly, would you be surprised?)
I take one that’s ‘take with 600 calories.’ Ok, as in, how close to eating? Before? After? What will happen if I’m not a nutritionist and therefore have NO IDEA how many calories will be enough? Do I need to whip out a food scale? Should I be doing math at breakfast? Is a bagel with cream cheese 600 calories or am I supposed to add a side of existential dread?
The Forgotten: Every medicine cabinet has them—the bottles in the back that you rediscover like archaeological artifacts. “Oh hey, I was supposed to be taking this for anxiety… six months ago. That explains a lot.”
I have a tough time with my late morning meds, so they often get forgotten until later in the day, then it’s the ‘would it be better to double up/take them closer to the night time ones? When do we no longer consider it because it’s too close to the others?’ Such fickle little things they are. It’s like playing medication Jenga—one wrong move and the whole system comes tumbling down.
The Systems I’ve Tried (And How They’ve Failed Me)
The Pill Organizer Approach: Seemed foolproof, right? Wrong. First, I had to figure out which size. The tiny ones where I can barely fit my horse-sized vitamins? The weekly ones that don’t account for my twice-daily medications? The monthly system that takes up half my kitchen counter?
I started out resisting these HARD, then went to the daily ones. They didn’t work—I’d forget to fill it, so one day at a time, I was not responsible enough for that. I lived, I learned, I got a weekly with the days broke into 4 sections, and it works. And if I forget, I always skip just because that’s easier to fix than the opposite way—it’s better to err on the side of caution. Nothing like turning medication management into a weekly game of Tetris.
The Phone Alarm Method: Set seventeen different alarms with helpful names like “ADHD Med” and “Don’t Forget Thyroid Pill.” Works great until you’re in an important meeting and your phone starts screaming “TAKE YOUR CRAZY PILLS NOW” at full volume.
Or, like me, you manage to dismiss them all subconsciously or your brain chooses to ignore them lol. It’s like my ADHD brain has developed selective hearing specifically for the alarms that are supposed to help me function. I can hear a bag of chips opening from three rooms away, but medication reminders? Nope, not registering.
The Medication Apps: Downloaded four different apps that promised to change my life. They all judged me harder than my mother when I inevitably forgot to log my doses. Nothing like a guilt trip from your phone to start the day.
The apps that would change my life all involved either purchases through the app, or require so much of my time I spent more energy journaling and entering the same responses than actually taking the medications. Or I’d not remember to enter them at all after week two. Apparently, I need an app to remind me to use the app that reminds me to take my medication. It’s apps all the way down.
The “I’ll Just Remember” Method: The most delusional approach of all. My ADHD brain that can’t remember where I put my keys five minutes ago was somehow going to remember a complex medication schedule. Spoiler alert: it didn’t work.
I will have my bottle in my hand wondering if I JUST took one, or if my brain is showing me past me taking them as I’d done countless times before. It’s like my brain is running a highlight reel of every time I’ve ever taken that medication, making it impossible to distinguish between “five minutes ago” and “Tuesday three weeks ago.”
The Real Struggles Nobody Talks About
The “Did I or Didn’t I?” Game: Standing in your bathroom at 2 PM, staring at a pill bottle, trying to remember if you took your morning medication or just thought really hard about taking it. It’s like the worst guessing game ever, with side effects as consequences.
So I stand there, debating my next move like it’s a choose-your-own-adventure novel: Option A: Take the pills and risk double-dosing myself into a nap I didn’t plan. Option B: Skip them and spend the rest of the day vibrating at the wrong frequency. Spoiler alert: I picked Option C — called my teen into the room and asked, “Hey, did you see me take these earlier?” They just stared at me like, “You realize I don’t follow your every move, right?” Thanks, kid. Very helpful.
The Pharmacy Mystery Calls: “Hi, your prescription for [medication you’ve never heard of] is ready for pickup!” Wait, what? When did I get prescribed that? Have I been supposed to be taking something this whole time?
Frequently I will go in for my appointment and bloodwork and she’ll call something in but forget to send the email until I contact them. So I’m left wondering if this mystery medication is something crucial I’ve been missing, or if it’s the pharmaceutical equivalent of a pocket dial. Either way, I’m driving to the pharmacy feeling like I’m solving a medical mystery.
The Coordination Nightmare: Doctor A wants to change medication X, but you have to check with Doctor B because it interacts with medication Y, and Doctor C doesn’t know about either of them because the medical records system is apparently held together with duct tape and prayers.
I once spent three weeks playing telephone between my psychiatrist, primary care doctor, and endocrinologist because nobody could agree on whether my new thyroid medication would interfere with my ADHD meds. Meanwhile, I’m sitting in the middle like a very tired, very caffeinated UN mediator, taking notes and trying to remember who said what about which pill. Spoiler alert: they all had different opinions, and I ended up being my own case study.
The Instruction Manual: That one medication that comes with a novel’s worth of instructions. Take with food, but not dairy. Don’t lie down for 30 minutes after taking. Avoid sunlight. May cause drowsiness or insomnia (thanks for being specific).
My personal favorite is the medication that says “may cause dizziness” and “do not operate heavy machinery,” but then also warns “may cause restlessness and inability to sit still.” So… I can’t drive, but I also can’t stop moving? Should I just pace around my house indefinitely? And don’t get me started on “take on an empty stomach” versus “take with food to avoid nausea.” Pick a lane, pharmaceutical industry!
What Actually Works (Sort Of)
After years of trial and error (emphasis on error), I’ve cobbled together a system that works approximately 73% of the time, which in my world counts as a rousing success.
My current system is that weekly pill organizer with four compartments per day, plus a backup system of keeping the bottles nearby for those “did I or didn’t I” moments and I actually write an x. I’ve learned to embrace the “when in doubt, skip it” philosophy because it’s easier to catch up on a missed dose than to undo a double dose. And yes, I still sometimes ask my family members if they’ve seen me take my pills, because apparently it takes a village to medicate one ADHD brain.
The key insight I’ve learned is this: there is no perfect system. There’s only the system that fails less catastrophically than the others. Some days I nail the medication schedule like a responsible adult. Other days I take my evening pills at 2 PM and wonder why I’m sleepy.
Just last week, I confidently took my morning pills, felt very proud of myself, and then found the same pills sitting in my pill organizer an hour later. Turns out I had taken yesterday’s forgotten dose. Mystery solved, but also… how did I not notice I was taking pills from the wrong day? ADHD brain strikes again.
The Bottom Line
If you’re struggling with medication management, know that you’re not alone in this pharmaceutical juggling act. We’re all just doing our best with brains that sometimes work against us and bodies that require more maintenance than a vintage car.
Your worth isn’t measured by how perfectly you follow your medication schedule. It’s measured by the fact that you keep trying, keep adapting, and keep finding ways to take care of yourself even when it feels impossibly complicated. Some days “good enough” really is good enough, and that’s perfectly okay.
Managing multiple chronic conditions isn’t just about remembering to take pills—it’s about being patient with yourself when your brain doesn’t cooperate, forgiving yourself when systems fail, and celebrating the small victories like remembering your evening meds before midnight.
Now if you’ll excuse me, I need to go stare at my pill bottles and try to remember if 2 PM counts as “evening” for my twice-daily medication.