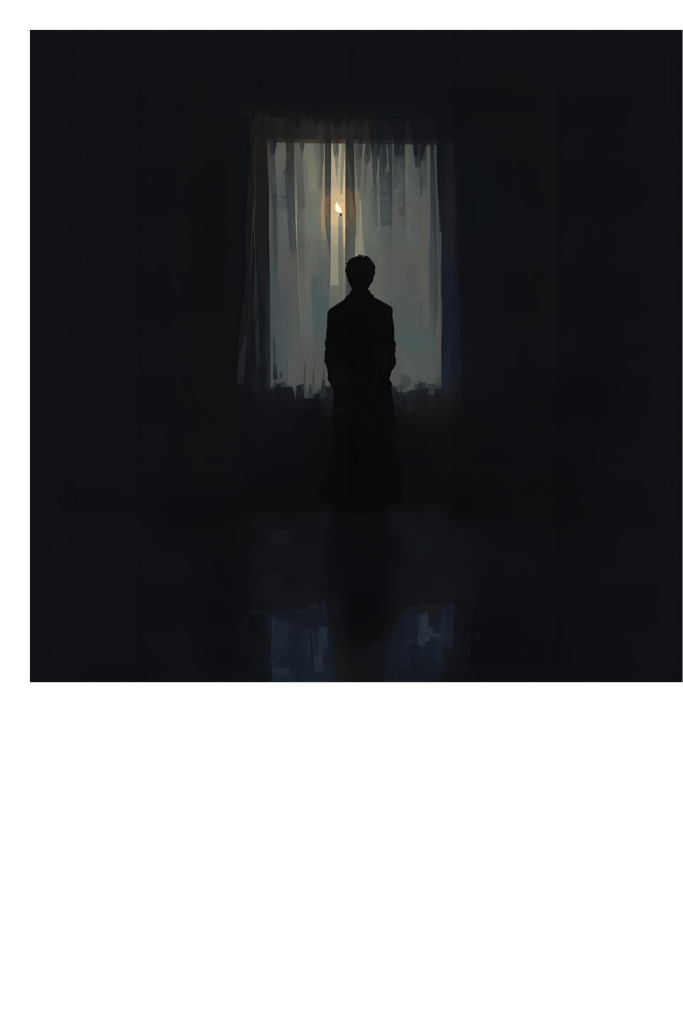
There’s a terrible little superpower I’ve developed: I can watch myself overreact.
It’s the worst seat in the house — front row, center stage — where my brain is performing a full-throttle disaster musical and I’m sitting there with the program, thinking, “Yep. That’s… dramatic.” Meanwhile my chest is doing interpretive dance, my throat is tight, and my hands have decided to be useless for the foreseeable future.

I know the script. I know the facts. I know that my kid is safe, that no one is angry enough to leave forever, that the noise outside is probably just traffic, not the arrival of doom. I can literally name the thoughts as they happen: This is a sign. This is going to spiral. Everyone will leave. I am unfixable. And I know, in a rational, calm part of my brain, that the thought is an alarm that’s been stuck on repeat. I also know that knowing it — intellectually — doesn’t flip a switch and make my body stop treating it like an emergency.
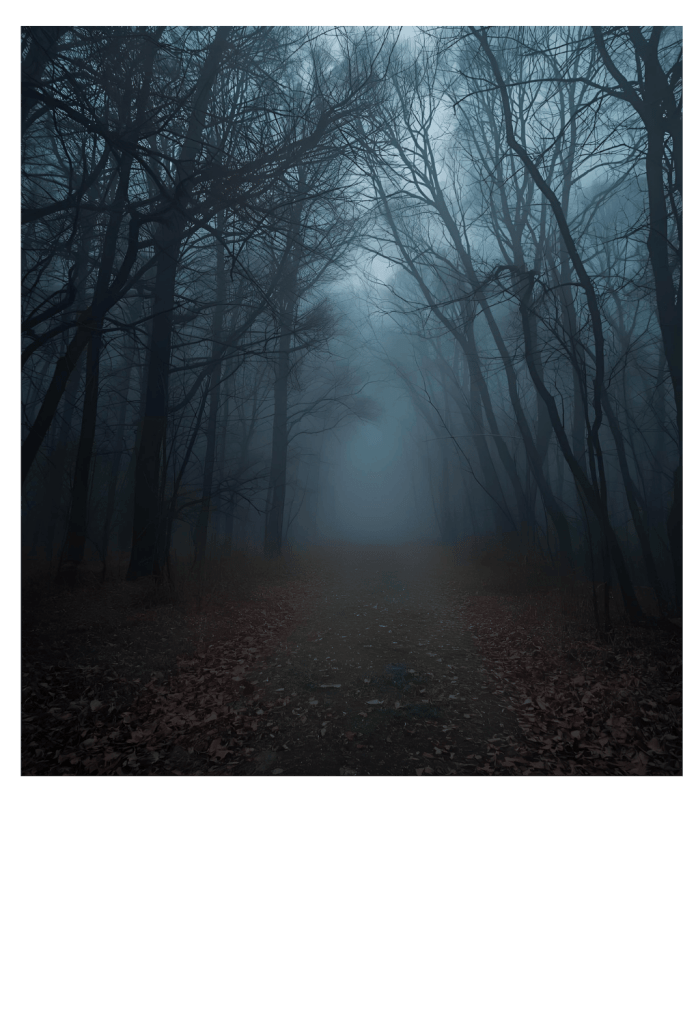
That’s PTSD after medical trauma for you in a sentence: your mind is both the actor and the audience. The rest of your life keeps going. You keep getting up, you keep making tea, you keep paying bills. But some invisible part of you stays backstage, rewinding and replaying a scary scene, making sound effects, and refusing to let the house lights come up.
Why the “I know it’s not true” feeling is its own kind of hell
It’s isolating. Because the knowledge that your thoughts are lying should be freeing, right? In theory. But being the person who can say, “This is irrational,” while your body screams “RUN” is exhausting and weirdly lonely. You end up apologizing to people for things they weren’t even upset about, or you cancel plans because you feel unsafe even though everything else says you’re fine. You blame yourself for being dramatic. You try to be the reasonable adult and the reasonable adult keeps getting ignored.
And then there’s guilt. If friends or family do help, you watch them pay attention and you feel both relieved and awful — because you think you’re costing them time and energy. You start to believe that self-sufficiency is the only moral option and asking for help is taking more than you deserve. Spoiler: that’s not the truth. It’s an emotional trap set up by fear.
Tiny, practical things that actually help when your brain runs the show
I’m not going to give you platitudes. Here are things that have helped me — small, honest, and doable even on the worst days.
- Label the play: When the alarm starts, say out loud (or mentally): “That’s my PTSD talking. That’s the survival brain.” Naming it doesn’t make it vanish but it takes away some of its power.
- Two-minute grounding: Five things you see, four things you can touch, three sounds, two smells, one thing you can taste (or one thing you like about the moment). It’s boring, and that’s the point. It pulls you out of the theater.
- Breathe like you mean it: 4-4-6 breathing (inhale 4, hold 4, exhale 6) calms the vagus nerve faster than a pep talk.
- Write the loop down: If a memory keeps looping, grab a notebook and write it until you’re bored of it. Then scribble one practical line: “Right now: I am home. Right now: I can breathe.” The page can hold the drama when your brain insists on replaying it.
- Micro-asks for people: Don’t make others guess. Say, “Can you sit with me for ten minutes?” or “Could you text me at 7 to check in?” People who care usually want the script — they just don’t want to mess it up.
- Make a tiny safety plan: three things to do if it spikes (call X, 2-minute grounding, favorite playlist). Tape it to the fridge if you have to. Pre-deciding reduces panic.
What to say — when you want to ask for help but hate feeling needy
Try something simple and specific:
“I’m feeling fragile today. I don’t need advice — could you just sit with me for 10 minutes?”
Or, if you need practical help:
“My energy is low; could you pick up milk on the way home? It would help more than you know.”
Short. Specific. Low drama. It gives people an easy yes.
The honest truth I remind myself (even when my brain screams otherwise)
I can hold two truths at once:
- My mind is telling a bigger story than the facts support.
- Needing help right now doesn’t make me a burden — it makes me human.
There’s a difference between the loudness of a feeling and the size of reality. Your feelings are not the final arbiters of truth. They are signals. Sometimes they’re reliable, sometimes they’re not. You don’t have to act on every alarm. You can notice it, honor it, and then choose what you do next.
A small support for the messy days

If you’re reading this while your chest is tight and your brain is staging a meltdown, I see you. I know how lonely it becomes to watch yourself react and feel like you’ve failed at being calm. You haven’t failed. You’ve survived things that rewired your alarm system. That makes your reactions loud — not your worth small. Til next time gang, take care of yourselves, and each other.