Your heart’s doing the cha-cha at 130 beats per minute. Your chest tightens. The world tilts. Your hands shake. Your brain starts whispering, “Hey, are we dying or just freaking out again?”
Is it POTS? A panic attack? A flashback to that one time your body really did betray you?
You’ve got about thirty seconds to figure it out before the anxiety of not knowing makes everything worse.
Welcome to the impossible diagnostic puzzle that is living with chronic illness and PTSD from medical trauma.
When Your Body Is Both the Scene of the Crime and the Witness
People with chronic illnesses are statistically more likely to develop PTSD-like symptoms—but the kicker is, it’s not from a one-time event. It’s because your body is an ongoing threat to your own sense of safety.
Unlike classic PTSD, where the trauma is technically in the past, medical PTSD means the trauma could literally happen again.
When you live with something like POTS, EDS, or MCAS, your body is both the suspect and the alarm system. The hypervigilance isn’t paranoia—it’s pattern recognition. You’ve learned that symptoms can mean something is seriously wrong.
But here’s the nightmare twist: those same symptoms—heart racing, shaking, dizziness—are also identical to a panic attack.
The Overlap That Makes You Want to Scream Into a Pillow
Let’s play a fun game called “Spot the Difference” between POTS and panic attacks:
POTS Symptoms:
- Rapid heart rate (120+ bpm)
- Dizziness or lightheadedness
- Shortness of breath
- Chest tightness
- Trembling, sweating, nausea
- Feeling like you might pass out

Panic Attack Symptoms:
- Rapid heart rate
- Dizziness or lightheadedness
- Shortness of breath
- Chest tightness
- Trembling, sweating, nausea
- Feeling like you might pass out
Yeah. Exactly the same.
So you sit there, pulse pounding, trying to decide if you need electrolytes or grounding exercises. And the longer you try to figure it out, the more anxious you get. Which—you guessed it—makes your heart race even more.
Congratulations, you’ve just triggered both conditions at once.
The “Is It My Body or My Brain?” Spiral
- Heart rate spikes.
- You think, “Is this POTS or panic?”
- The uncertainty feeds the anxiety.
- Anxiety makes your heart rate climb higher.
- PTSD brain jumps in like, “Hey, remember the last time this happened?”
- Your body floods with stress hormones.
- Symptoms worsen, clarity vanishes, and you’re stuck in a full-body loop of chaos.
Sometimes grounding doesn’t work. Sometimes standing makes it worse. Sometimes everything makes it worse. The mental gymnastics of self-triage would exhaust an Olympic athlete, and that’s before you even factor in the fatigue that both conditions bring.
When Hypervigilance Isn’t a “Coping Issue”
In classic PTSD, hypervigilance—constantly scanning for danger—is something therapy tries to reduce.
But when you live with a chronic condition that can cause fainting, cardiac issues, or anaphylaxis, that vigilance might literally save your life.
So how do you tell your brain to “calm down, you’re safe” when sometimes… you actually aren’t?
This is the impossible bind of trauma plus illness:
PTSD therapy says, stop monitoring every sensation.
Your medical team says, monitor every sensation.
Neither is wrong. Neither fully works.
The Medical Gaslighting Cherry on Top
And just to make it more fun: when you do seek help, you get hit with the “it’s just anxiety” script.
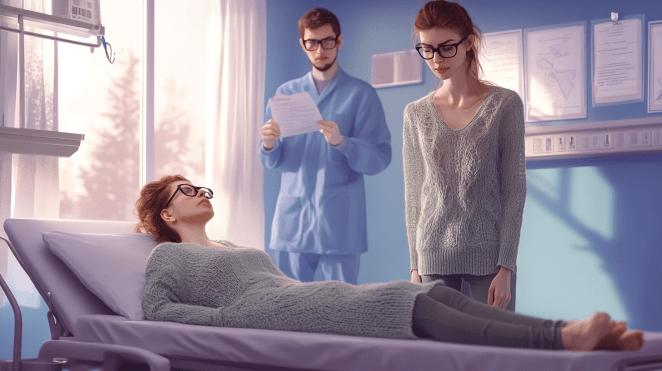
Even though POTS isn’t caused by anxiety, and even though research shows anxiety rates are about the same as the general population, you’ll still have doctors waving off your physical symptoms because your chart says PTSD.
You start to lose faith in professionals. You stop asking for help. You learn to rely only on yourself for triage—because nobody else seems capable of telling the difference either.
Which means you’re back to square one, again, sitting in the impossible space of trying to figure it out alone.
The Treatment Contradiction
PTSD therapy often involves exposure work—facing the thing that scares you until your brain chills out about it.
Except in this case, the “thing that scares you” is your own body.
You can’t just take a break from having a body. You can’t “gradually reintroduce” the experience of dizziness or tachycardia when those things are daily realities that might require medical intervention.
Worse, some PTSD therapies intentionally raise your heart rate to help you practice staying calm through physical sensations. That’s great… unless you have POTS, where that heart rate spike might actually make you faint.
So you end up in a no-win situation where treating one condition can trigger the other.
What Actually Helps (Sometimes)
There’s no perfect fix here. But there are ways to soften the edges:
💡 Look for patterns, not moments. Track triggers over time. Are symptoms linked to posture, temperature, dehydration, or specific memories? Zooming out can help reduce panic in the moment.

💡 Build a “both/and” plan. Sit down? Yes (helps POTS). Ground yourself? Yes (helps panic). You don’t have to guess which one it is to respond with compassion instead of chaos.
💡 Find trauma-informed doctors. You need providers who understand that your nervous system and your medical symptoms aren’t separate universes.
💡 Accept uncertainty. Sometimes you just won’t know—and that’s not failure. That’s reality.
💡 Validate yourself. You’re not dramatic. You’re not broken. You’re reacting appropriately to a wildly confusing body situation that most people can’t imagine.
The Unspoken Truth
Living with medical PTSD and chronic illness means constantly trying to interpret a body that lies to you and tells the truth at the same time.
It means your hypervigilance is both too much and not enough.
It means your body is both the warning sign and the danger.

You’re not failing to cope—you’re surviving something that isn’t designed to make sense.
And honestly? That’s nothing short of heroic.
Til next time, gang, take care of yourselves, and each other!
🧠 Research Toolbox
- American Psychological Association. Medical trauma and PTSD in patients with chronic illness (2020).
- Raj, S. R. (2022). Postural Orthostatic Tachycardia Syndrome (POTS): Pathophysiology, Diagnosis, and Management. Cleveland Clinic Journal of Medicine.
- Löwe, B. et al. (2021). Trauma, PTSD, and chronic illn