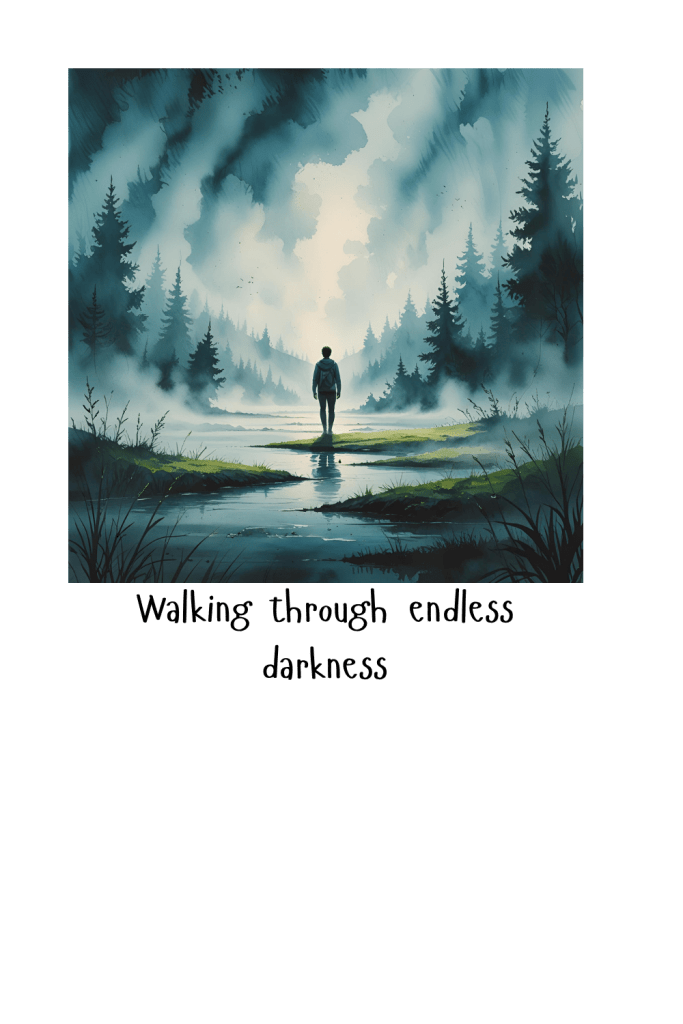
There are moments when I’m technically awake, technically functioning, but not really here.
I’ll be mid-sentence and lose the sentence. Mid-thought and lose the thought. Mid-day and suddenly it’s hours later.
That’s dissociation — and it’s a lot quieter, weirder, and more common than people think.
This isn’t a dramatic shutdown. It’s not a panic attack. It’s not giving up.
It’s my nervous system quietly saying: this is too much right now.
What Dissociation Actually Feels Like
Not the textbook version. The real-life one.
- My body keeps going, but my brain feels like it stepped out for coffee.
- Sounds feel slightly delayed, like everything is happening behind glass.
- Emotions flatten — not sad, not calm, just muted.
- I forget what I’m saying while I’m saying it.
- Time skips. Ten minutes disappears. Sometimes an hour.
It doesn’t feel scary in the moment — it feels empty. And that’s often what makes it unsettling afterward.
Why It Happens (No Jargon, I Promise)
Your brain has two big jobs:
- Keep you alive
- Process information and feelings
When stress, pain, trauma, sensory overload, or emotional pressure stack too high, the brain makes a call:
“Processing everything right now would cost too much energy.”
So it pulls back.
Less sensation. Less emotion. Less memory formation.
This isn’t a flaw. It’s a conservation strategy.
How to Gently Come Back (Without Forcing It)
Dissociation doesn’t respond well to yelling at yourself to focus.
It responds to safety cues.
1. Start With the Body
Thinking your way out rarely works — the body has to go first.
- Press your feet into the floor and notice the pressure
- Wrap up in a hoodie or blanket (weight helps)
- Hold something textured: a mug, fabric seam, stone
Feeling your body is the bridge back.
2. Use Temperature as a Reset

Temperature changes speak directly to the nervous system.
- Splash cool water on your face
- Hold something warm or cold in your hands
- Step outside for fresh air if you can
You’re telling your body: we’re here, and it’s now.
3. Name What’s Happening
No analysis required.
Quietly acknowledging it helps reduce fear:
- “I’m dissociating right now.”
- “My system is protecting me.”
- “I don’t have to fix this — just notice it.”
Naming brings orientation without pressure.
4. Ground Through One Sense (Not Five)
Sometimes the classic five-senses exercise is too much.
Try just one:
- Sight: name one color you can see
- Sound: listen for the furthest noise you can hear
- Touch: rub your thumb across your fingers slowly
Simple works better than intense.
5. Externalize Memory When Words Slip
If thoughts are falling through trapdoors:

- Write a single keyword
- Record a 10‑second voice memo
- Text yourself: “brain offline — continue later”
This isn’t failure. It’s accommodation.
Aftercare Matters More Than You Think
When dissociation fades, what often shows up next is shame.
Why can’t I just stay present?
But dissociation means something was already overwhelming.
The kind response is not pushing harder — it’s softer transitions:
- water
- food
- low stimulation
- rest
You don’t need to earn recovery.
One Last Thing
Dissociation doesn’t mean you’re bad at coping.
It usually means you’ve coped a lot.

Your nervous system learned this because it once helped you survive.
Now you’re teaching it that there are other safe options too.
And that learning takes time.
Gentle time. Til next time gang, take care of yourselves, and each other.










 What Dissociation Actually Is
What Dissociation Actually Is
 But What Does That Look Like as a Parent?
But What Does That Look Like as a Parent?
 What Helps Me Come Back
What Helps Me Come Back
 If This Is You Too…
If This Is You Too…